Best Casino Tips at Casino Moons: Login Australia, Get Free Chips, Free Spins, Withdrawal Guide, and Honest Review
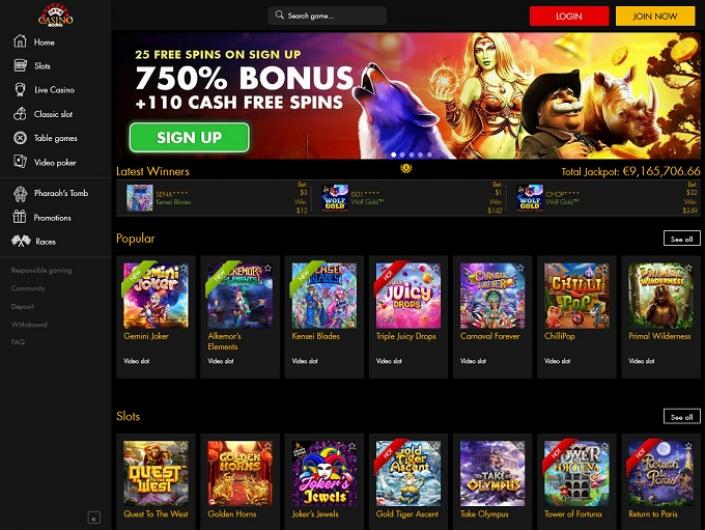
Welcome to the ultimate guide to mastering your experience at Casino Moons, the online casino that has become a buzzword in gaming circles, especially in Australia. As we embark on this comprehensive journey, we’ll delve into the essentials of navigating the Casino Moons platform. From the ease of login process for Aussie players to the excitement of claiming your Casino Moons free chip 2024, each aspect is carefully explored to enhance your gaming adventure.
In this Casino Moons review, we’ll walk you through various facets of this casino. You’ll learn about the seamless login process, making it a breeze for players Down Under to get started. Additionally, we will shed light on how to maximize the benefits of the free chips, a perk that sets this platform apart in the competitive world of online casinos.
Casino Moons Ease of Access in Australia
Casino Moons has carved a niche in the Australian online gaming market, known for its user-friendly access and diverse range of slot games. Here’s a closer look at why it stands out:
- Ease of Logging In: The Casino Moons login Australia process is designed with simplicity in mind. It ensures that players from Australia can start their gaming journey with minimal fuss. This accessibility is a key reason why many Australian gamers prefer Casino Moons.
- Diverse Slot Options: After completing the Casino Moons login Australia procedure, players are greeted with an impressive array of slot games. Casino Moons takes pride in its variety, offering everything from classic slots to modern video slots.
- Regular Updates: Keeping the gaming experience fresh and exciting, Casino Moons slots are regularly updated. This ensures that players have access to the latest and most popular titles in the online slot world.
- Seamless Integration: The integration of Casino Moons slots with the overall casino interface is seamless. This allows for an uninterrupted gaming experience, where players can easily switch between different slot games without any hassle.
- Accessibility Across Devices: Whether you’re playing on a desktop or a mobile device, the accessibility remains consistent. This multi-device compatibility ensures that players can enjoy their favorite Casino Moons slots anytime, anywhere.
- Support System: If players encounter any issues during the Casino Moons login Australia process or while playing slots, the platform’s customer support is readily available to assist, making the experience hassle-free.
- Promotions and Bonuses: The platform frequently offers promotions and bonuses, particularly on Casino Moons slots, enhancing the overall gaming experience for players.
Casino Moons stand out in the Australian online casino market due to its easy login process and diverse range of slot games. The platform’s focus on accessibility, variety, and player convenience makes it a top choice for Australian players.
Indulge in Generous Free Chips 2024

Casino Moons has become a haven for players who love extra value, and their generous free chip offers are a testament to this. Delving into the world of free chips at Casino Moons reveals:
- Initial Welcome Bonus: New players are often greeted with a Casino Moons free chip as part of their welcome package. This initial bonus serves as a great introduction to the casino’s offerings and a chance to explore games without immediate investment.
- Regular Player Rewards: Not just for newcomers, regular players can also enjoy the Casino Moons free chip 2024 offers. These are typically available through ongoing promotions, loyalty programs, or special events.
- Variety of Games: The Casino Moons free chip 2024 can be used across a diverse range of games. From slots to table games, players have the freedom to explore different gaming experiences without dipping into their deposited funds.
- Easy Claim Process: Claiming a Casino Moons free chip is straightforward. Whether it’s through a promotional code or automatic crediting, the casino ensures that players can easily access their free chips.
- Transparent Terms: Casino Moons maintains transparency in its terms and conditions regarding the use of free chips. Players are encouraged to understand these terms to maximize their benefit from the Casino Moons free chip.
- 2024 Updates: Looking ahead, Casino Moons is poised to continue offering the with even more exciting features and benefits, keeping the player experience fresh and rewarding.
The Casino Moons free chip 2024 is a cornerstone of the gaming experience at Casino Moons, offering both new and regular players a chance to enhance their gameplay. Whether used as a strategic tool or simply to enjoy a broader range of games, these free chips add significant value to the overall casino experience.
Spin and Win: Free Spins Galore
Free spins are a highlight for any slot enthusiast, and Casino Moons excels in offering these delightful bonuses. Let’s explore how free spins Casino Moons enriches the gaming experience:
- Welcoming Free Spins: As part of the welcome package, free spins Casino Moons extends an invitation to new players to spin and win. These spins are a fantastic way to get acquainted with the casino’s diverse slot offerings without any initial investment.
- Diverse Slot Selection: The free spins can be used across a wide array of slot games, showcasing Casino Moons’ commitment to variety. From classic fruit machines to modern video slots, there’s a game for every taste.
- 50 Free Spins Offer: The Casino Moons 50 free spins promotion is a standout offer. This generous number of spins allows players to substantially engage with the games, increasing their chances of winning.
- Regular Promotions: Besides the welcome offer, regular promotions keep the excitement alive. Free spins Casino Moons often includes free spins in their weekly or monthly promotions, keeping players engaged and rewarded.
- Loyalty Rewards: Loyal players aren’t left out. They can earn Casino Moons 50 free spins or more through loyalty programs, which often reward players based on their gaming activity.
- No Deposit Required: Some free spin offers, like the Casino Moons 50 free spins, may not even require a deposit, making them accessible to a broader range of players.
In summary, free spins Casino Moons is a cornerstone of the Casino Moons experience, offering both new and regular players a chance to explore a wide range of slots, risk-free. Whether through welcoming new players or rewarding the loyalty of existing ones, these free spins add an extra layer of excitement and opportunity to the gaming experience.
Understanding Casino Moons Withdrawal Process
A smooth withdrawal process is crucial in online casinos, and Casino Moons has streamlined its system to ensure a hassle-free experience. Here’s a detailed look at the Casino Moons withdrawal process:
- Simple Withdrawal Steps: The process for Casino Moons withdrawal is straightforward and user-friendly. Players can easily navigate through their accounts to find the withdrawal option, ensuring a smooth transition from playing to cashing out.
- Verification for Security: To ensure the safety of funds, Casino Moons requires a verification process during the first withdrawal. This step is crucial for protecting both the player and the casino and maintains the integrity of the Casino Moons withdrawal process.
- Withdrawal Limits and Times: Understanding the limits and expected time frames for withdrawals is key. The Casino Moons withdrawal guidelines clearly outline minimum and maximum limits, as well as processing times, helping players plan their cash-out strategies.
- Utilizing Bonus Codes: Players who have used Casino Moons no deposit bonus code must pay attention to the wagering requirements associated with these bonuses. These requirements need to be met before initiating a withdrawal to ensure a smooth process.
- Multiple Payment Methods: Casino Moons offers a variety of payment methods for withdrawal, catering to a wide range of preferences. Whether it’s bank transfers, e-wallets, or other options, players can choose the most convenient method for them.
In conclusion, understanding the withdrawal process is vital for a seamless online gaming experience. From the simple steps to cash out to the importance of meeting wagering requirements from Casino Moons bonus codes, players are equipped with all the necessary information for a smooth withdrawal process. With an emphasis on security, convenience, and transparency, Casino Moons ensures that players can enjoy their winnings with peace of mind.
Exclusive Bonuses and Promotions
Casino Moons stands out for its attractive bonuses and promotions, designed to enhance the gaming experience for every player. Let’s delve into the world of Casino Moons bonus codes and the exclusive offers available:
- Range of Bonus Codes: The variety of Casino Moons bonus codes available is impressive. These codes can unlock different types of bonuses, from match deposits to free spins, catering to a wide range of player preferences.
- No Deposit Bonuses: A highlight is the Casino Moons no deposit bonus code. This particular code allows players to receive a bonus without the need to make an initial deposit, providing a risk-free way to enjoy the games.
- Easy Access to Bonuses: Claiming bonuses using Casino Moons bonus codes is a straightforward process. Players can easily enter the codes in the designated area and enjoy the benefits that come with them.
- Regularly Updated Offers: Casino Moons keeps its promotions fresh by regularly updating its Casino Moons bonus codes. This ensures that players always have something new and exciting to look forward to.
- Loyalty Rewards: Beyond the initial welcome bonuses, regular players can benefit from loyalty programs. These programs often use Casino Moons bonus codes to reward frequent players with exclusive bonuses.
The bonuses and promotions at Casino Moons, accessible through Casino Moons no deposit bonus codes, offer a dynamic and rewarding experience for players. These bonuses not only enhance the gameplay but also provide opportunities to enjoy more games and potentially win more, all while ensuring a fair and transparent gaming environment.
A Vast Array of Slot Games

Casino Moons prides itself on offering a wide and varied selection of slot games, ensuring an engaging experience for every kind of player. This section explores the depth and diversity of Casino Moons slots and how they’re enhanced by free spins.
- Expansive Selection: The Casino Moons slots collection encompasses a range of themes, payouts, and play styles. From classic three-reel slots to the latest video slots, there’s something to satisfy every taste and preference.
- Continual Updates: Casino Moons regularly updates its Casino Moons slots portfolio. This means players are always treated to the latest and most innovative games in the market, keeping the gaming experience fresh and exciting.
- Free Spin Integrations: Many of the Casino Moons slots come with integrated free spin features, allowing players to extend their playtime and increase their chances of winning. These free spins often come as part of the game itself or through various promotions.
- High-Quality Graphics and Sound: The slots at Casino Moons boast high-quality graphics and immersive soundtracks. This attention to detail ensures an enjoyable and engaging gaming experience across all Casino Moons slots.
- Special Features and Bonuses: Many slots offer special features like bonus rounds, multipliers, and wilds, adding an extra layer of excitement and opportunity for players.
- Accessibility: Whether on desktop or mobile, Casino Moons slots are accessible across various devices, ensuring players can enjoy their favorite games anytime, anywhere.
- Fair Play: Casino Moons is committed to fair play, with all Casino Moons slots using Random Number Generators (RNGs) to ensure unbiased outcomes.
The array of Casino Moons slots is a significant draw for players, offering a mix of traditional and modern games with various themes and features. The added benefit of free spins Casino Moons promotions makes the platform even more enticing, providing numerous opportunities for players to enjoy and potentially win big. Whether you’re a seasoned slot enthusiast or new to the world of online slots, Casino Moons has something to offer for everyone.
Conclusion
Our comprehensive exploration of Casino Moons concludes, but the excitement and opportunities it offers continue. This Casino Moons review has delved into various aspects of the platform, highlighting its strengths and the experiences it offers to players, particularly in Australia.
- A Comprehensive Gaming Experience: Casino Moons has successfully created a gaming environment that combines variety, excitement, and user-friendliness.
- A Hub for Slot Lovers: The vast selection of Casino Moons slots and the generous offers of free spins Casino Moons stand out as major attractions. These features not only provide entertainment but also enhance players’ chances of winning.
- User-Friendly Withdrawal Process: When it comes to financial transactions, the Casino Moons withdrawal process is streamlined and transparent, ensuring that players can easily access their winnings with minimal hassle.
- Security and Fair Play: Throughout this Casino Moons review, it’s clear that the platform prioritizes security and fair play, ensuring a safe and trustworthy environment for all its players.
Casino Moons offers a well-rounded, enjoyable, and secure online gaming experience, making it a highly recommended platform for both new and experienced players. As always, we encourage responsible gaming and wish you the best in your future gaming endeavors at Casino Moons.